Chimeric Antigen Receptor T cells (CAR-T)
Chimeric Antigen Receptor T-cell (CAR-T) therapy, represents a significant advancement in cancer treatment, particularly in the realm of immunotherapy. This innovative approach involves the genetic modification of a patient’s T cells to enhance their ability to recognize and attack cancer cells. The process begins with the extraction of T cells from the patient’s blood, followed by engineering these cells to express chimeric antigen receptors (CARs) that specifically target tumor-associated antigens. Once modified, these CAR-T cells are reinfused into the patient, where they proliferate and mount an immune response against the cancer.
CAR-T cell therapy involves several key steps to modify a patient’s T cells to effectively target and destroy cancer cells
1.T Cell Collection: T cells are harvested from the patient’s blood through a procedure called leukapheresis.
2.Genetic Modification: The collected T cells are genetically engineered in a laboratory to express chimeric antigen receptors (CARs).
3.Cell Expansion: Once the T cells are modified, they are cultured in the lab to multiply.
4.Reinfusion: The engineered CAR-T cells are infused back into the patient.
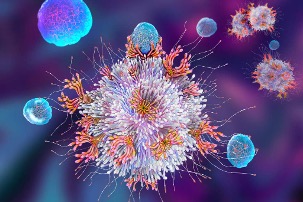
5.Targeting Cancer Cells: Once in the body, the CAR-T cells circulate and recognize cancer cells by binding to the specific antigen targeted by the CAR.
Memory Formation: After the initial attack, some CAR-T cells become memory T cells, which can persist long-term and provide ongoing surveillance against cancer recurrence.
